Upper Limb Rehabilitation in Chronic Stroke
A Research Study Opportunity
Researchers from Baylor Scott & White Institute for Rehabilitation and the Texas Biomedical Device Center (TxBDC) at The University of Texas at Dallas have teamed up to assess if implanted vagus nerve stimulation (VNS) coupled with rehabilitation is able to improve recovery of arm function after a stroke. Therapy will take place over six weeks and follow-ups will occur at 1, 3, and 6 months after therapy ends. Participants will be compensated for their time in the study.
Key Eligibility Requirements
- Must have had an ischemic stroke that occurred 12 months or more prior to enrollment.
- Must be between the ages of 22 and 79 years.
- Must demonstrate some arm and hand movement.

For more details, contact Alvaro Carrera at 469-831-5321 or email alvaro.carrera@bswhealth.org.

Learn more about the Baylor Scott & White Research Institute.
Frequently Asked Questions
What is the purpose of the trial?
Researchers from Baylor Scott & White Research Institute and the Texas Biomedical Device Center at The University of Texas at Dallas have teamed up to assess if implanted vagus nerve stimulation (VNS) is able to improve recovery of arm function after a stroke.
What activities does the trial involve?
Before enrollment in the trial, participants will go through a few steps to determine if they are eligible to be in the trial. First will be a call with a trial staff member to go over basic information and a brief set of questions to determine if they seem like a good fit for the study. If they are, the participant will be scheduled for an initial visit to go over and sign the consent form. After consenting to the study, there will be a more in-depth assessment to find out if the participant can continue in the study; this is called screening and will be in person with the trial’s chief medical officer and other trial staff.
If eligible, participants will be enrolled in the study and scheduled for surgery to implant the device. About two weeks after surgery, participants will receive physical therapy at the same time vagus nerve stimulation is delivered. The vagus nerve stimulation does not hurt. Many participants are not expected to feel it at all. Questionnaires and clinical assessments of movement and sense of touch will be completed before and after six weeks of therapy.
How long is the surgery?
The surgery involves one small incision on the left side of the neck and is expected to take about 60 minutes.
Is the surgery done with general anesthesia?
Yes. Participants will be asleep during surgery.
How long is recovery?
After surgery, study participants will recover for about one week.
How do I care for the incision?
The incision should be kept covered until it has healed and is evaluated at the post-op visit.
What is the device and system?
The system is called the ReStore System. It consists of a very small vagus nerve stimulator that sits on the vagus nerve in the neck and two devices used to trigger the vagus nerve stimulation: 1) the Power and Communication Device (PCM) and 2) the study phone. The PCM is worn outside the skin in a neckband and powers, communicates with, and controls the implanted device. The study phone programs and controls the VNS device. This device is investigational and not FDA approved.
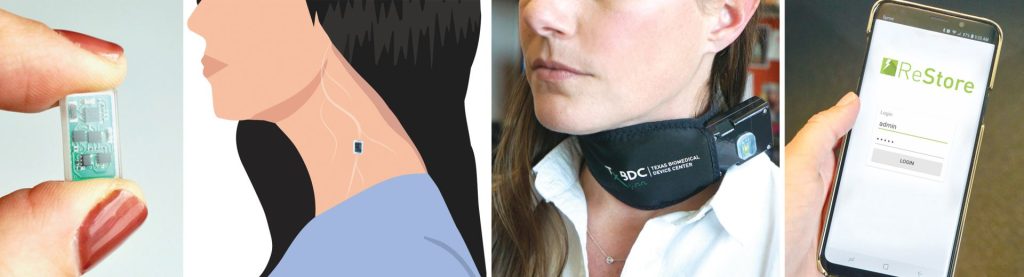
Does the neckband have to be worn at all times or just during therapy?
The neckband is only worn during therapy sessions which are one hour long.
Where is the trial taking place?
The trial will take place at the Baylor University Medical Center and Baylor Scott & White Institute for Rehabilitation in Dallas.
How often do the visits take place?
Visits are weekly for the first month. Once therapy begins, there will be three visits per week for six weeks. Each session will be approximately an hour long.
What kind of assessments are involved?
Questionnaires and clinical measurements of movement and sense of touch will be completed by study staff.
How does the therapy work?
The therapy is designed to increase the number of neural connections responsible for movement and touch.
When will this therapy be coming to a clinic near me?
Currently, the therapy is only available as part of an FDA-approved clinical trial. The therapy will take at least two years to complete the necessary testing for final approval.